Ever had that feeling where your food seems to just sit in your stomach? That discomfort could be gastroparesis. It’s a condition where the muscles in your stomach don’t work right, making it hard to move food into your small intestine. Numerous unpleasant symptoms may result from this. If you’ve been diagnosed with gastroparesis, you might see codes like “K31.84” or “E11.43.” These are ICD-10 codes, a system doctors and insurance use to classify diagnoses. But what do these codes mean for you?
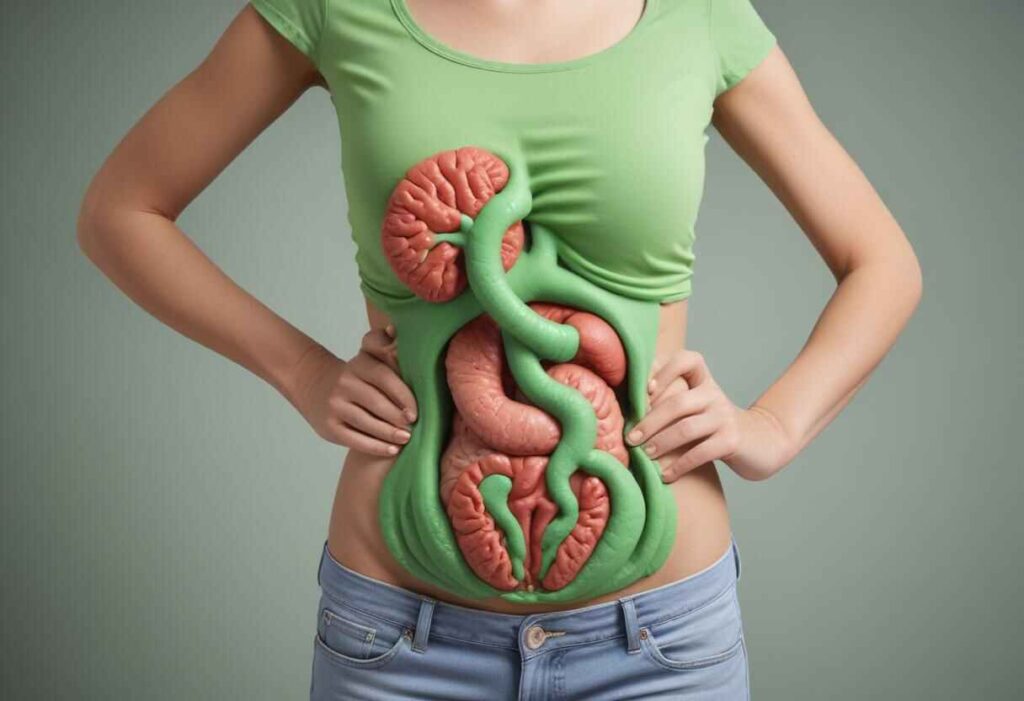
What is Gastroparesis?
In a healthy digestive system, the stomach muscles push food into the small intestine for further digestion. However, in people with gastroparesis, the stomach muscles don’t work properly, so food stays in the stomach too long. This delay can disrupt normal digestion and nutrient absorption, and in severe cases, it can lead to malnutrition and dehydration.
Decoding the Code
There are two main ICD-10 codes for gastroparesis:
- K31.84: This code is used for gastroparesis itself, indicating the presence of the condition.
- E11.43 (with autonomic neuropathy): This specific code is used when gastroparesis is caused by nerve damage related to diabetes (autonomic neuropathy). Since diabetes often leads to gastroparesis, this code helps show the underlying cause.
ICD-10 Code for Gastroparesis

The International Classification of Diseases, Tenth Revision (ICD-10), is a system for coding and classifying diseases. The ICD-10 code for gastroparesis is K31.84. Healthcare providers and insurers use this code to record and bill for medical services related to gastroparesis.
Detailed Explanation of ICD-10 Code K31.84
K31.84 is the ICD-10 code for gastroparesis. Here’s how it fits into the coding system:
- K00-K93: Diseases of the digestive system.
- K20-K31: Disorders affecting the duodenum, stomach, and oesophagus.
- K31: Other duodenal and stomach disorders.
Within the K31 category, K31.84 is specifically for gastroparesis. This code helps doctors and insurers document, track, and bill for treatment accurately.
Causes of Gastroparesis
The exact cause of gastroparesis is often unknown, but several factors can lead to it:
- Diabetes: High blood sugar can harm nerves, including those in the stomach that control muscle movement.
- Post-Surgery: Some abdominal surgeries can damage nerves or muscles that help the stomach work properly.
- Medications: Certain medicines, like painkillers or antidepressants, can affect how stomach muscles contract, leading to gastroparesis.
- Idiopathic: Sometimes, the exact cause of gastroparesis is unknown, which is called idiopathic gastroparesis.
- Other Health Conditions: Conditions such as Parkinson’s disease, multiple sclerosis, or hypothyroidism can also contribute to gastroparesis.
Symptoms of Gastroparesis
Gastroparesis, which means “stomach paralysis,” is a condition where the stomach takes too long to empty its contents into the small intestine. Symptoms can vary and may include:
- Nausea and Vomiting: Feeling sick to your stomach or throwing up, especially after eating.
- Feeling Full Quickly: Getting full soon after you start eating, even if you haven’t eaten much.
- Bloating: Feeling swollen or uncomfortable in your abdomen.
- Abdominal Pain: Having pain in your belly, which can be mild or strong.
- Heartburn or Acid Reflux: Feeling a burning sensation in your chest (heartburn) or stomach acid coming back up into your throat.
Diagnosis of Gastroparesis
Gastroparesis is usually diagnosed using a combination of medical history, physical examination, and tests. Here’s how doctors typically diagnose it:
- Medical History: Your doctor will ask about symptoms like nausea, vomiting, feeling full quickly, bloating, and stomach pain. They’ll also ask about any conditions you have, such as diabetes or past surgeries.
- Physical Examination: During a physical exam, the doctor will check your abdomen for tenderness, listen for bowel sounds, and look for signs of malnutrition or dehydration.
- Blood Tests: These tests can measure electrolyte levels, kidney function, blood sugar (especially if diabetes is suspected), and overall nutrition.
- Imaging Tests: You might get an abdominal X-ray or ultrasound to rule out other issues and check for blockages or abnormalities.
- Gastric Emptying Study: This test is key for diagnosing gastroparesis. You eat a meal with a bit of radioactive material and then get scans over a few hours to see how fast your stomach empties.
Treatment and Management
While there is no cure for gastroparesis, several treatments can help manage its symptoms and improve quality of life:
- Dietary Changes: It can be beneficial to eat smaller, more frequent meals and to select foods that are readily digested. Avoid high-fat and high-fiber foods.
- Medications: Medicines like metoclopramide and erythromycin can help stomach muscles contract. Anti-nausea medications can also relieve symptoms.
- Medical Procedures: In severe cases, treatments like gastric electrical stimulation or feeding tubes may be needed to ensure proper nutrition.
Living with Gastroparesis
Managing gastroparesis often requires both medical treatment and lifestyle changes. Regular check-ups with doctors, following dietary advice, and taking medications properly are very important. Help from dietitians, gastroenterologists, and support groups can also greatly improve the lives of those with this condition.
Conclusion
Gastroparesis is a difficult condition that impacts daily life. Knowing its causes, symptoms, and treatment options is key to managing it well. The ICD-10 code K31.84 helps doctors and insurers identify and document gastroparesis, improving communication and treatment planning. With the right care and support, people with gastroparesis can live healthier and more comfortable lives.
Visit Here: ICD-10-CM Codes
